What is Viral Hepatitis A?
Viral hepatitis A is a benign acute cyclic viral infection from the group of fecal-oral hepatitis, accompanied by necrosis of hepatocytes. It is clinically manifested by intoxication syndrome, hepatosplenomegaly and often jaundice. Synonyms – Botkin’s disease, viral hepatitis type A.
For the first time the idea of the infectious nature of “catarrhal jaundice” expressed JV. Botkin (1888); Since that time, the disease has long been called “Botkin’s disease.” In 1947, F. McCollum proposed the term “hepatitis A”; the causative agent was discovered much later (S. Finestone, 1973).
Causes of Viral Hepatitis A
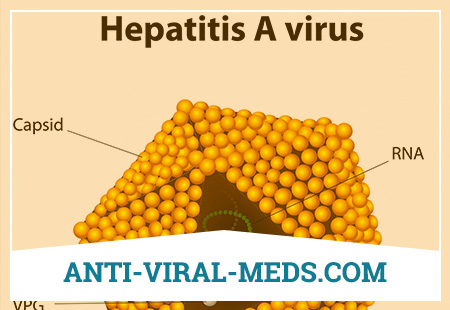
The causative agent of viral hepatitis A is an RNA genomic virus of the Hepatovirus genus of the family Picornaviridae. Virions are small, simply arranged, devoid of supercapsid. The genome is formed by single-stranded RNA. Currently, only one virus serovar is known. In the external environment, it is more resistant than typical enteroviruses. May persist in the environment for several months at 4 ° C, for several years at – 20 ° C, for several weeks at room temperature. The virus is inactivated by boiling after 5 min. Under ultraviolet irradiation, the pathogen dies after 60 s. In the presence of chlorine in a concentration of 0.5-1 ml / l, at pH 7.0, it survives 30 minutes or more, which determines its ability to persist for a certain time in chlorinated tap water.
The reservoir and source of infection is a person with any manifestations of the disease (icteric, anicteric, asymptomatic and inapparent forms). A significant part of the infected suffers the disease in an asymptomatic, and therefore unreported form. In children, this value reaches 90-95%, in adults – 25-50%. A sick person is dangerous to others from the 2nd week of the incubation period of the disease; peak virus excretion occurs in the first week of illness. Contagiousness of the patient with the appearance of jaundice is significantly reduced: in the first week of the icteric period, the frequency of positive findings is 30-50%, in the second – 15-25%, later the isolation of the virus is observed only in individual patients. Chronic carriage of the virus is not installed. Cases of human infection from chimpanzees and some other monkey species are described.
The transmission mechanism is fecal-oral. Virus isolation occurs with fecal masses. In 1 ml of feces can contain up to 108 infectious virions. Infection of people occurs through the use of water and food infected with a virus, sometimes by contact-household means. Discusses the possibility of sexual transmission of infection, especially among homosexuals. In a number of countries (USA, European countries), cases of diseases associated with infection by the parenteral administration of psychotropic substances, blood transfusion and its drugs are described. The role of each transmission path varies in different conditions. The waterway usually leads to outbreaks of the disease among people using infected water, swimming in polluted pools and lakes. Since the virus of viral hepatitis A can survive in water from 12 weeks to 10 months, infection can occur when eating various raw mollusks, mussels collected in areas polluted by sewage.
Food outbreaks are most often associated with contamination of products in food enterprises by personnel with a mild form of the disease, with non-compliance with the rules of personal hygiene. It is also possible contamination of vegetables and berries (especially strawberries and strawberries, lettuce) when they are fertilized with human feces. Contact-household transmission, as a rule, takes place in the conditions of pre-school institution, children’s homes and other similar institutions, especially in the conditions of their poor sanitary condition.
Human natural susceptibility is high. After the infection has been transferred, a persistent, intense immunity is produced. The most susceptible children are from 2 to 14 years old. Asymptomatic forms of the disease form a less stressful immunity.
Major epidemiological signs. Viral hepatitis A is distinguished by its widespread distribution, uneven intensity in certain territories, cyclicality in perennial dynamics, pronounced autumn-winter seasonality, predominant affection of preschool children, adolescents and young people.
Viral hepatitis A is among the most widespread intestinal infections in the world. Of all the numerous forms of viral hepatitis, it is most often encountered. WHO reports approximately 1.4 million cases of viral hepatitis A reported annually. On average, direct and indirect costs due to infection can reach $ 2,459 per case for an adult and $ 1,492 for a child. The costs associated with viral hepatitis are estimated annually in the world from 1.5 to 3 billion US dollars.
Although this disease is mainly characteristic of third-world countries with low levels of hygiene and sanitation, isolated cases or outbreaks of viral hepatitis A can be observed even in the most developed countries. In the United States, it is estimated that about 33% of the population has serological markers that indicate an infection. 143 thousand cases of infection with viral hepatitis A are celebrated annually.
The incidence of children with hepatitis A virus is constantly higher than in adults. The age of 3–6 years determines the level of child morbidity, the rate among them in 1998 was 82.7 per 100,000 of the population, in 1999 – 77.0. The incidence among the urban and rural population is almost equal, the figures are respectively 30.0 and 32.6 per 100,000 population.
In 1999, 14,152 studies of environmental objects on antigens of the viral hepatitis A virus were conducted, of which 474 (3.4%) were positive; The greatest number of positive results was obtained in the study of water from sources of decentralized water supply (9.6%) and faecal waste water (6.4%). This indicates a wide circulation of the pathogen in the external environment with the development of outbreaks mainly of water origin in regions with poor sanitary and communal condition.
For long-term dynamics, the presence of periodic (after 4-6 years) increases in incidence is characteristic. The most recent years characterizes the next rise in incidence. A feature of the last rise was the emergence of epidemic outbreaks with food transmission.
The summer-autumn seasonality of morbidity is noted, which reflects a pronounced increase in the importation (importation) of infection from disadvantaged areas with migration flows of the population and the supply of various low-quality food products sold in conditions of wholesale and unauthorized (street) trade. Among adults, workers at all catering establishments, as well as the nutrition and treatment centers of medical, children’s, sanatorium and other institutions, are primarily at risk of contracting viral hepatitis A. Military personnel and persons leaving or residing in the territory unsuitable for sanitary-communal use, using water from open reservoirs for household purposes, as well as medical personnel are additionally referred to the high-risk group. In recent years, people with chronic liver and biliary tract diseases, homosexuals and drug addicts have been ranked as risk groups, since among them are described group cases of viral hepatitis A.
Pathogenesis During Viral Hepatitis A
The mucous membranes of the oropharynx and small intestine are the usual entry gates for the viral hepatitis A virus. An inflammatory process develops at the site of introduction that causes the formation of a catarrhal syndrome, dyspeptic phenomena and a temperature reaction. Penetration of the pathogen into the blood leads to viremia, through which it reaches the liver. It is currently assumed that damage to hepatocytes is due to cellular cytotoxic immune responses. However, do not exclude the direct cytopathic effect of the virus on hepatocytes. In patients with viral hepatitis A, liver biopsy revealed significant damage to the portal area with intense cellular infiltration and destruction of the border plate, and marked signs of cholestasis.
Even with a small lesion of hepatocytes, hepatolienal syndrome forms, biliary dyskinesia develops; with more severe liver damage, jaundice occurs. In the future, it takes several weeks to restore hepatocytes, and several months to restore complete cytoarchitecture of the liver.
The antigens of the viral hepatitis A virus exhibit high immunogenicity: activation of the immune system and specific sensitization of lymphocytes begin with the introduction of the pathogen.
Virus antigens (envelope proteins) are expressed on hepatocyte membranes in a complex with antigens of the main histocompatibility complex (HLA) type I, and infected cells are destroyed by cytotoxic T lymphocytes and T-killers.
The similarity of virus antigens and hepatocyte antigens determines the development of common autoimmune processes, the intensity of which largely determines the outcome of the disease. Persons with a genetic predisposition due to viral hepatitis A may develop chronic autoimmune type I hepatitis. Nephrotic syndrome with the development of mesangioproliferative glomerulonephritis, arthritis, vasculitis, cryoglobulinemia; at the same time viral hepatitis A acted as a provoking factor. In very rare cases (0.1%) fulminant forms of viral hepatitis A may develop.
Already during the incubation period, specific IgM are detected; the duration of the incubation is explained by the individual features of the immune response. With the rapid increase in antibody titers, jaundice does not develop.
As a result of immune reactions in most cases, rather quickly, within 2-3 weeks, recovery occurs with the complete release of the body from the virus. The virus infection and chronic forms of viral hepatitis A are not observed.
Symptoms of Viral Hepatitis A
The incubation period lasts 3-4 weeks. Viral hepatitis A occurs as an acute cyclical disease and is characterized by a successive alternation of several periods — prodromal (dojelous), height (icteric), and the period of convalescence.
Dozheltushny period. It is characterized by a fairly wide variety of symptoms, conditionally grouped in several variants of its course.
- Influenza-like (febrile, catarrhal) variant in viral hepatitis A is most common. Usually, the disease begins quite acutely with an increase in body temperature (from subfebrile to high numbers), weakness, malaise, muscle pain, the development of lung catarrhal symptoms (nasal congestion, pain or sore throat, cough). However, flu-like symptoms in most patients are accompanied by dyspeptic disorders of varying severity.
- Dyspeptic option. Catarrhal phenomena are absent, and symptoms of gastrointestinal tract involvement come to the fore. Patients are disturbed by discomfort in the epigastric region, loss of appetite until complete anorexia, nausea, and sometimes vomiting, which occurs more often after eating. There may be dull pain in the right hypochondrium, bitter taste in the mouth, belching, constipation, or loose stools.
- Asthenovegetative option. It is characterized by a number of non-specific symptoms: the development of general weakness, loss of working capacity, irritability or indifference, persistent insomnia, or, conversely, drowsiness.
Viral hepatitis A can clinically manifest immediately with the development of jaundice; in this case, prodromal signs are absent (latent variant of the initial period).
It should be emphasized that clinical symptoms related to different variants of the dozheltushny period can be combined in various combinations. In these cases, talking about the mixed version.
Complications of Viral Hepatitis A
Develop relatively rarely. These include exacerbations of inflammatory processes in the biliary tract (cholecystitis, cholangitis, dyskinesias), as well as the development of secondary infections (pneumonia, etc.). Acute hepatic encephalopathy in viral hepatitis A is extremely rare.
Diagnosis of Viral Hepatitis A
Diagnosis of viral hepatitis A in its initial period is extremely difficult. It is necessary to rely on the data of the epidemiological history (contact with icteric patients). When examining patients already at this time, it is possible to detect an enlarged liver and an increase in the indices of aminotransferases.
The initial period of the disease lasts from 2 to 7-10 days and gradually turns into jaundice. At this point, the temperature reaction normalizes, catarrhal phenomena disappear, but dyspeptic symptoms persist or even may increase in intensity.
The onset of the icteric period must be counted from the moment the dark urine appears. Following this, icterus appears on the bridle of the tongue, soft palate, sclera, and then on the skin. Its intensity progresses rapidly, usually reaching a maximum in 3-4 days; at the same time jaundice often gets a saffron shade. It is believed that the intensity of jaundice is directly proportional to the severity of the disease, however, it is necessary to focus more on the severity of intoxication syndrome: repeated vomiting, dyspeptic disorders, degree of loss of appetite. With a more severe course of the disease on the skin can be noted the appearance of bruises, especially at the injection sites. In some patients, nosebleeds are observed.
Language, as a rule, is imposed. Palpatorno determine enlarged liver, sensitive to palpation; the degree of its increase may be different. In 30-40% of cases by this time splenomegaly is found. In some patients in the midst of jaundice appears bleached stools. On the part of the cardiovascular system, bradycardia and a tendency to lower blood pressure are quite characteristic. On the background of jaundice, in addition to dyspeptic phenomena, patients note adynamia, dizziness, and sometimes sleep disorders.
The duration of the icteric period in viral hepatitis A does not exceed 30 days. More often, it lasts about 2 weeks and goes into a period of recovery. By this time there is a gradual decrease in the intensity of the icteric syndrome, the liver is reduced in size, signs of intoxication disappear. The recovery period is significantly longer than the period of jaundice, and can be delayed up to 3-6 months.
In 5-10% of patients with viral hepatitis A may acquire a longer course, characterized by small manifestations or lack of intoxication, small numbers of bilirubinemia and hyperfermentemia, a persistent increase in liver size. Most often this explains the development of cholestasis. Despite the increased duration of the disease ends favorably.
Viral hepatitis A usually occurs in mild or moderate forms, but severe variants and exacerbations are not excluded.
Diagnosis of viral hepatitis A is mainly carried out with a pronounced icteric syndrome, however, a large number of reports have accumulated that viral hepatitis A can often occur in the form of anaicum, which in most cases is not diagnosed. According to some researchers, the ratio of icteric and anicteric forms can reach 3: 7.
In the pre-jaundice period viral hepatitis A, it is necessary to carry out differential diagnostics with acute respiratory and intestinal infections. The epidemiological anamnesis data can provide some assistance in differential diagnosis: contact with icteric patients, patient’s stay in areas unsuccessful in hepatitis A. In some cases, an enlarged liver can be detected in the pre-jaundice period, as well as an increase in the activity of aminotransferases.
In the icteric period, the disease is differentiated from obstructive and hemolytic jaundices, mononucleosis, yersiniosis, leptospirosis. The clinical picture, in many respects similar to the listed diseases, requires the determination of hepatitis markers using ELISA and PCR, the determination of bilirubin and its fractions in the blood.
Laboratory diagnosis
Laboratory studies are of particular importance to establish the etiology of hepatitis and assess its severity. In the analysis of blood, it is necessary to take into account the presence of leukopenia, relative lymphocytosis and slowing of ESR.
The intensity of jaundice is determined on the basis of determining the level of bilirubin in the blood (especially its bound fraction). The activity of aminotransferases [alanine aminotransferase (ALT) and aspartate aminotransferase (ACT)] increases several times, and the degree of its increase indicates the intensity of hepatocyte cytolysis. Violations of the liver protein synthesizing function reflect changes in the indices of colloidal samples (decrease in sublimate and increase in thymol samples), a decrease in the level of albumin and prealbumin in the blood, as well as a decrease in the prothrombin index.
Virus hepatitis A can be isolated from faeces, but virological studies are not used in general medical practice. For verification of the diagnosis, serological reactions are used – ELISA, RIA, revealing an increase in specific IgM in the icteric period and an increase in IgG titers by the period of reconvalescence. The most reliable diagnostic method is the detection of virus RNA in the blood by PCR.
Treatment for Viral Hepatitis A
After establishing the fact of viral hepatitis A disease, the patient can be treated on an outpatient basis. Patients are hospitalized with a severe course of the disease, protracted forms, in the presence of severe concomitant diseases, as well as persons of the prescribed groups.
Patients are prescribed bed rest for the period of pronounced intoxication syndrome and good nutrition. In the diet, refractory fats, difficult-to-digest meats (lamb, pork, waterfowl), fried foods, canned food, pickles, onions, garlic and spices are excluded. Alcohol is strictly prohibited. Recommended milk and vegetable food. Additionally, vitamins of groups C and B are added to food products.
In connection with the lack of etiotropic therapy, pathogenetic treatment is carried out. To remove intoxication, depending on its degree, use abundant drink or infusion solutions. For daily bowel cleansing and suppression of anaerobic flora, it is recommended to prescribe lactulose derivatives, the doses of which are selected individually. For the relief of the cholestatic component, antispasmodics (no-spa, euphylline) and ursodeoxycholic acid derivatives are used.
After completion of the disease, the patient is subject to follow-up at 3-6 months.
Prevention of Viral Hepatitis A
The main measures to prevent infection with viral hepatitis A are to provide the population with benign water and to create conditions that guarantee the implementation of sanitary rules for the preparation, storage, preparation and sale of food. It is of great importance to ensure proper anti-epidemic regime in organized children’s and adult groups. In the fall (high-risk time), they should acquire the character of anti-epidemic: in particular, preschool education institutions and school institutions, even in the absence of diseases, should be considered as potential foci of viral hepatitis A. Actions should be directed to actively searching for sources of infection, including identifying IgM in ELISA, strengthening disinfection regime, subject sanitary education of children and adults in relation to the real danger of infection with viral hepatitis A. In the period of pre-season increase in the incidence of effective immuno lobulinoprofilaktika providing protection for 3-4 months. Vaccination coverage of 50-60% of children of the UDU and 70-80% of schoolchildren ensures a reduction in the incidence in these groups by 2-3 times. Children of preschool age are administered 0.75 ml immunoglobulin, primary school children 1.5 ml, older children and adults, depending on their weight, up to 3 ml. The introduction of immunoglobulin is allowed no more than 4 times during life with an interval of not less than 1 year.
Currently, a vaccine against viral hepatitis A has been proposed as a means of specific prophylaxis, since the administration of immunoglobulin provides quick but short-term protection. Vaccinal prophylaxis forms an active immunity accompanied by a prolonged circulation of its own antibodies. They produce effective and harmless vaccines against viral hepatitis A for children and adults, ensuring the preservation of immunity up to 10 years. However, the widespread vaccination against viral hepatitis A is hampered by its relatively high cost. However, it is known that the damage caused by viral hepatitis A, far exceeds the cost of vaccination. Considering the high susceptibility of children and the fact that they are the main source of infection for adults, vaccine prevention of viral hepatitis A in young children and schoolchildren, widely held in the United States and several countries (Israel, Spain), is a promising direction.
Vaccines are formalin-inactivated viral hepatitis A virions adsorbed on aluminum hydroxide. They are administered intramuscularly. The vaccine is used in children from 3 years and adults. Adults vaccine is administered in a dose of 0.5 ml in the deltoid muscle. Course – 3 vaccinations according to the scheme of 0, 1 and 6 months. Children injected with 0.25 ml in the deltoid muscle twice with an interval of 1 month. Avaxim vaccine (France) is administered to children from 2 years old and adults once intramuscularly, revaccination is carried out 6–18 months once, subsequent revaccination is every 10 years. Vaccine Vaccine (USA) is administered from 2 years of age as a single primary dose (for children 25 antigenic units – 0.5 ml, for adults 50 antigenic units – 1 ml) with a repeated dose in 6-18 months. Havriks vaccine (Belgium) is used in children from 1 year old and in adults. Available in 0.5 ml ampoules (720 U) for children and 1 ml (1440 U) for adults.
Vaccination stimulates the development of immunity in 21-28 days. Antibody titers, although lower than after the disease, provide reliable protection against infection.